Hong Kong News

Dental internship plan not finalised, Hong Kong health chief says after criticism
Hong Kong’s health chief has sought to clarify a controversial government proposal requiring dental graduates to work at public institutions, saying it only meant to ask them to fulfil a one-year internship and had not decided whether to make staying on afterwards compulsory.
Secretary for Health Lo Chung-mau on Sunday did not commit to whether the scope of public dental services would be expanded with the roll-out of the new requirement after critics argued the proposal might only help civil servants as existing care at government clinics largely benefited them.
“Let’s not let certain arguments focus on what we can do purely on the civil service. The civil service does not have a gap right now. The most important issue is that we can help the disadvantaged by filling the gap,” he told a television programme aired on Sunday.
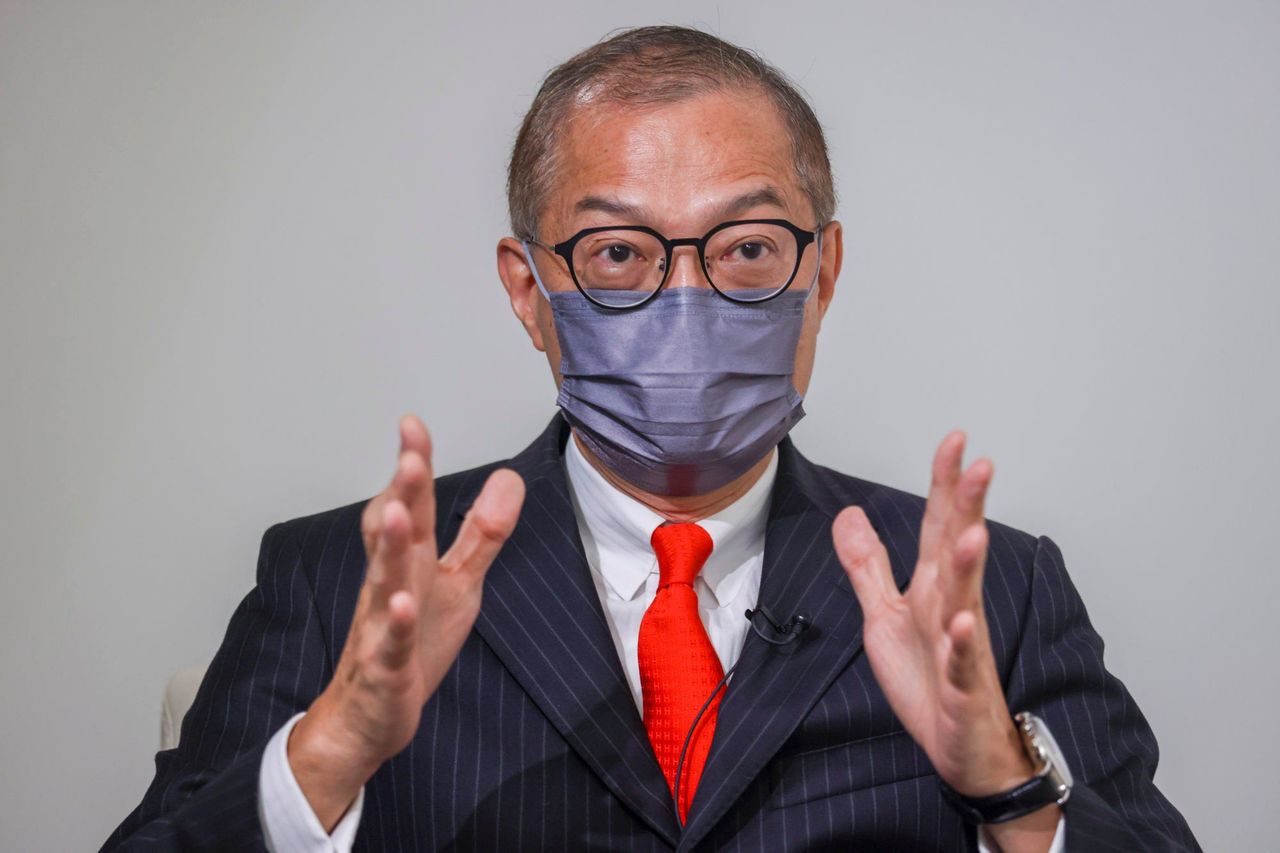 Secretary for Health Dr Lo Chung-mau.
Secretary for Health Dr Lo Chung-mau.
Currently, dental students have to finish six years of academic training, including clinical sessions. Under the proposal revealed by the sector, graduates will have to undergo a one-year internship at a designated public health clinic before they can register as dentists and then stay there for another two years.
Lo said there had been no decision on whether the government would make it mandatory for dentists to work for two years in public health after their one-year internship.
He argued it was not too much to ask a dentist – when the government had spent about HK$3 million (US$382,302) on each for their training – to work in the public sector for three years because they typically spent 35 years in the industry after graduation.
“If we are calculating based on three years [working in the public sector], it will account for less than 9 per cent of their professional career. The impact is not very big,” he said.
“But we also considered the problems if we increase the number of years. We will take [the proposal] as a starting point for discussion.”
He said out of 2,706 registered dentists in Hong Kong, nearly 10 per cent of them had gone overseas, while 45 per cent were reaching retirement age.
The shortage was severe, Lo said, pointing to the Department of Health’s nearly 100 vacancies. The new measures should be implemented as soon as possible, he said.
Addressing questions on whether doctors would also have similar arrangements, Lo said there was no timetable to implement measures for them.
“Doctors currently have to undergo internship for one year,” he said, adding that close to 80 per cent of doctors had joined public medical institutions for specialist training, which took six years.
“Of course, we have to discuss with the industry, especially medical schools, whether we want them to stay longer after the specialist training, this is the next step.”
Medical and health services sector lawmaker Dr David Lam Tzit-yuen said the measure should be a “last resort”, adding the government should offer more details on how it would like to provide extensive dental healthcare to the general population first before deciding how to increase manpower.
“[The government] must let us know what kind of public services they are going to expand and what is the timeline of providing the services to the public … how much resources will they invest on these services and what sort of facilities and equipment are they going to acquire,” he said.
“Then we can decide if we can import more dentists or ask [existing] local dentists to stay longer. If that doesn’t work then we can make it compulsory and require dental graduates to stay.”
Chief Executive John Lee Ka-chiu said in his policy address last year that the government would look into different options to ensure sufficient manpower at healthcare facilities, including requiring workers to serve in public institutions and admitting qualified non-locally trained professionals.
Authorities set up the Working Group on Oral Health and Dental Care in December to follow up on Lee’s proposal.
The proposal had earlier sparked concern among leaders in the dental industry, as they questioned whether it would benefit residents or dental students.
About 316 dentists in Hong Kong work in public clinics, which provide check-ups for primary school children and elderly residents with health vouchers.
Public dental health services do not cover secondary school students, while elderly residents queuing overnight for appointments is a common sight in the city.
The working group has been tasked with reviewing the scope of public dental services, including providing more targeted care for underprivileged groups and high-risk patients. It will also devise a long-term strategy to secure more workers and coordinate service programmes.











