Hong Kong News

About 16 per cent of Hong Kong’s young people have likely mental problem: study
More than 16 per cent of Hong Kong’s young people have a probable psychiatric disorder, with family relationships and lack of private space identified as a major risk factor, an unprecedented mental health study of thousands of teenagers carried out in the city has found.
And experts on Thursday appealed to health authorities to tackle the impact that rapid digitalisation and artificial intelligence have had on the mental health of youngsters and to boost their ability to face the problems and opportunities of the hi-tech era.
Researchers discovered close to 20 per cent of respondents had suicidal thoughts in the last 12 months, 5 per cent had made a plan to take their own lives and 1.5 per cent had attempted suicide.
“Those demonstrating major depressive disorder are three times more likely to have suicidal thoughts and eight times more likely to make a suicide plan and attempt,” said Professor Eric Chen Yu-hai, the chair professor in the University of Hong Kong’s psychiatry department.
“It is therefore an important screening item in suicide prevention.”
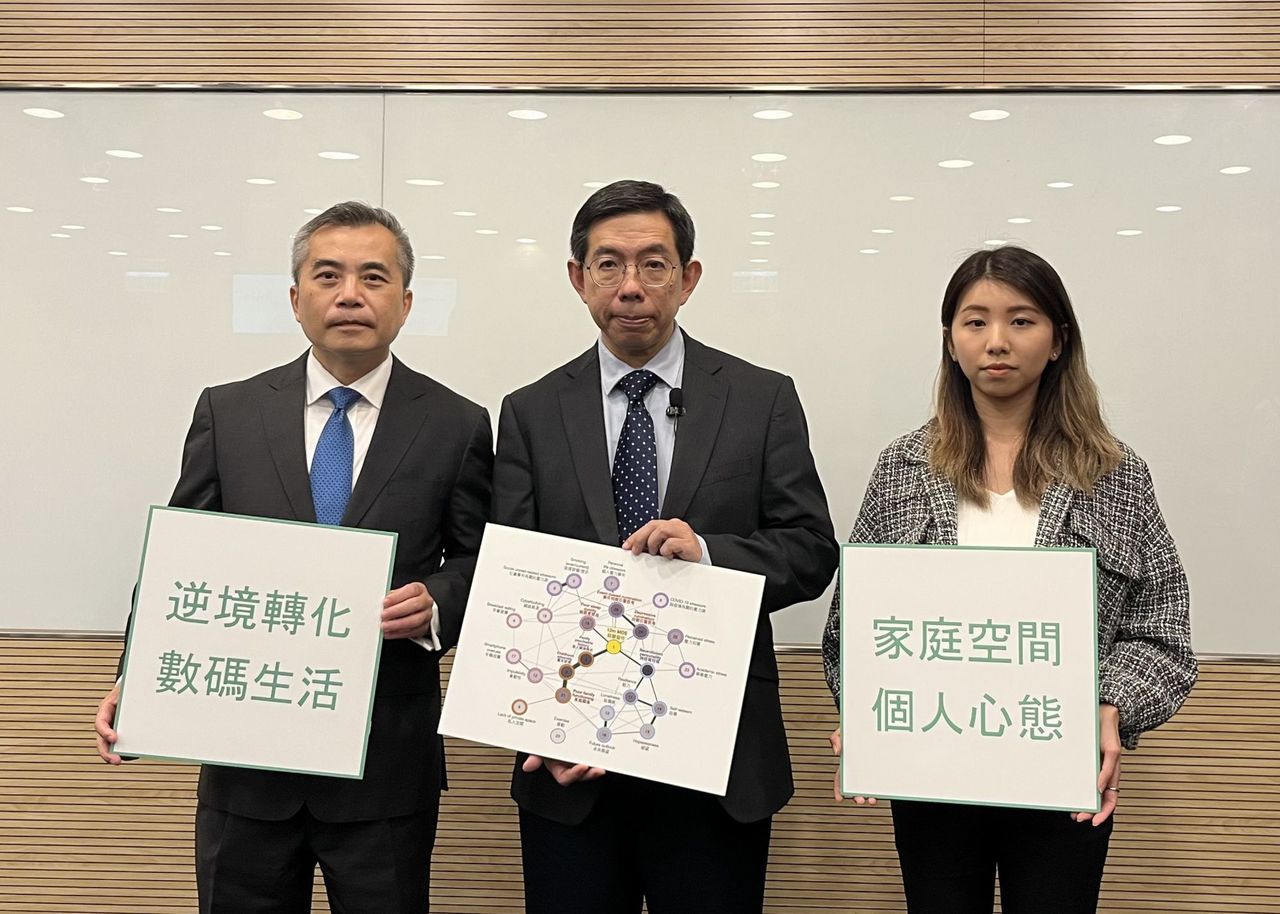 Wong Yan-lung, chairman of the Advisory Committee on Mental Health
(left), with Professor Eric Chen, HKU psychiatry department’s chair
professor, and Dr Stephanie Wong, a research officer with the
department.
Wong Yan-lung, chairman of the Advisory Committee on Mental Health
(left), with Professor Eric Chen, HKU psychiatry department’s chair
professor, and Dr Stephanie Wong, a research officer with the
department.
He was speaking after a team from the university’s psychiatry department interviewed 3,340 youngsters aged 15 to 24 between 2019 and 2022, using a random sampling approach, to gauge how widespread psychiatric disorders were.
The research team, which worked with the government’s Census and Statistics Department, sent out invitations to the addresses of potential participants and carried out multiple face-to-face and online interviews.
Interviews with clinicians were arranged for those with psychotic disorders and other participants whose mental health was at risk.
The study, commissioned by the city’s health authorities, found that the prevalence of probable mental disorders among teenagers, including major depressive episodes, bipolar, psychotic, anxiety, and panic disorder, was 16.6 per cent, with depression being the most common condition.
Depression was found to be most prevalent among women aged 22 to 24 who also lived in public rental housing.
But researchers discovered almost 75 per cent of young people with mental disorders had not had any psychiatric and psychological support, attributed by some respondents to the long waiting lists for services.
Hospital Authority figures earlier showed the median wait for new stable cases at public psychiatric clinics was 40 weeks, with more than 38,000 people in the queue.
Chen said some participants had to wait for two years to be seen by a professional and had lost the motivation to get treatment.
He added others were unwilling to accept help for mental health problems because they feared they would be stigmatised.
The study also revealed that academic stress was the biggest source of worry, followed by work and concerns over personal lives.
Researchers identified four major risk factors, with “family and space” the biggest, in a bid to help the health service better target its resources.
Youngsters with a family history of psychiatric problems, childhood difficulties, poor family relationships and a lack of personal space were found to be more likely to suffer from poor mental health.
Dr Stephanie Wong Ming-yin, a research officer at the department, said more than 30 per cent of respondents admitted they could not discuss their feelings with their families and 16 per cent felt they did not have enough support at home.
Chen emphasised the importance of more spaces for youngsters to relax, as many participants in the study had struggled to find privacy for their online interviews, especially during Covid-19 lockdowns.
He added another important factor was “stressor and coping” as the entire population had faced huge strains from a variety of sources in recent years, including the Covid-19 pandemic, the emigration wave and a weak economy.
“Those major events are impacting the younger generation as they are at a critical stage of their life,” he said.
“Some youngsters would start to ruminate about these stressors, which are both uncontrollable and unsolvable, and that subsequently resulted in worse mental health.”
 Mental health experts have appealed to health authorities to tackle the
impact that rapid digitalisation and artificial intelligence have had on
the mental health of youngsters.
Mental health experts have appealed to health authorities to tackle the
impact that rapid digitalisation and artificial intelligence have had on
the mental health of youngsters.
He said a targeted approach to get them out of a negative thinking loop, including cognitive-behavioural therapy and mindfulness-based treatments, was needed.
The other two factors were the digital lifestyle, which included an unhealthy use of smartphones that often resulted in poor sleep quality and breakfast skipping, as well as poor mentalities, such as lower resilience, poor self-esteem, and impulsive behaviour.
“The family factor is persistent and can hardly be changed, but the personal mentality, digital habits, as well as their ways to cope with external challenges are controllable,” Chen said.
He advised young people to start with small lifestyle changes, such as eating breakfast every day, to help improve their mental health.
But Chen said he believed that an era of rapid change which had led the young to question their self-worth was the driving force behind the four risk factors.
“We are entering the age of information and intelligence, but are we ready to cope with the changes?” he asked.
“With the help of technology, our life is more convenient and we can have information at our fingertips, but what exactly do we need and how can we position ourselves when AI seems to be replacing us?”
He said it was important that a humanistic approach was taken as the government pushed forward with the idea of a smart city and that the potential of people should be factored in.
Wong Yan-lung, the chairman of the Advisory Committee on Mental Health, said psychiatric well-being was linked to contextual changes, which society had to accept, and were unavoidable.
“As new challenges emerge, it’s crucial to identify the risk factors, which were the root causes, and respond with a new set of strategies and mindset accordingly,” Wong said.
“Equipping the younger generation with such ability is what the government, families and all relevant stakeholders should work on.”
The university team said it wanted to continue to track changes in the mental health of survey participants and carry out similar large-scale studies in the future.











